Risk-based monitoring (RBM) is a clinical trial monitoring approach that focuses resources on areas that pose the greatest risk to data quality and patient safety. The RBM approach is gaining popularity as it provides a more efficient and effective method for monitoring clinical trials. However, implementing RBM can be a challenging task. Following are the 12 benefits of RBM:
- Increased efficiency: RBM is a more efficient approach to monitoring clinical trials, as it allows monitoring resources to be focused on critical areas of the trial, rather than monitoring all data points. This can lead to reduced monitoring time and effort, allowing resources to be directed to other aspects of the trial.
- Cost savings: RBM can be more cost-effective than traditional monitoring, as it allows for resources to be focused on critical areas, reducing the need for excessive monitoring activities and unnecessary travel. This can lead to significant cost savings in terms of monitoring resources and expenses.
- Improved data quality: By focusing on critical data points, RBM can improve the quality of data collected, ensuring that it is accurate, complete, and consistent. This can lead to more reliable study results, and help to reduce the risk of errors and omissions.
- Enhanced patient safety: RBM allows for potential safety risks to be identified and addressed early on, improving patient safety and reducing the risk of adverse events. This can help to ensure that patients are protected throughout the trial, and that potential safety risks are identified and addressed proactively.
- Better risk management: RBM allows for a more comprehensive risk management approach, with potential risks identified and addressed proactively. This can help to reduce the risk of errors and omissions, and ensure that potential issues are addressed before they become major problems.
- More targeted monitoring: RBM allows for monitoring activities to be tailored to the specific trial and risk profile, ensuring that resources are focused on the most critical areas of the trial. This can help to reduce monitoring time and effort and ensure that monitoring resources are directed where they are most needed.
- Faster query resolution: RBM can lead to faster resolution of data queries, as potential issues are identified and addressed early on in the trial. This can help to reduce delays in data collection and analysis, and ensure that study timelines are met.
- Increased compliance: RBM can improve compliance with regulatory requirements, as potential issues are identified and addressed proactively. This can help to ensure that the trial is conducted in accordance with regulatory requirements and that potential compliance issues are identified and addressed before they become major problems.
- Improved communication: RBM requires effective communication and collaboration among stakeholders, improving communication and transparency throughout the trial. This can help to ensure that all stakeholders are aware of potential issues, and that potential issues are addressed proactively.
- More effective resource allocation: RBM allows for resources to be allocated more effectively, ensuring that resources are focused on the most critical areas of the trial. This can help to reduce resource waste, and ensure that resources are directed where they are most needed.
- Increased transparency: RBM allows for greater transparency throughout the trial, with potential issues identified and addressed proactively. This can help to ensure that all stakeholders are aware of potential issues, and that potential issues are addressed in a transparent and collaborative manner.
- Better trial outcomes: By improving data quality, patient safety, risk management, and compliance, RBM can lead to better trial outcomes and more reliable study results. This can help to ensure that the trial meets its objectives, and that study results are accurate and reliable.
In summary, implementing RBM in clinical trials can lead to a variety of benefits, including increased efficiency, cost savings, improved data quality, enhanced patient safety, better risk management, more targeted monitoring, faster query resolution, increased compliance, improved communication, more effective resource allocation, increased transparency, and better trial outcomes. These benefits can help to ensure the success of clinical trials, improving patient outcomes and advancing medical research.
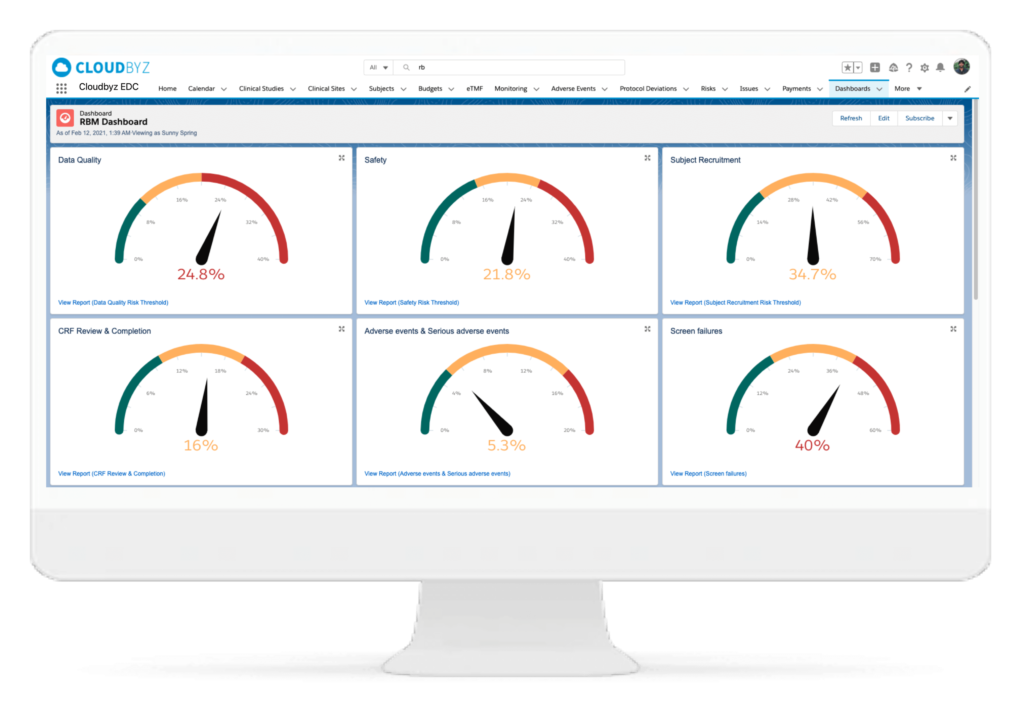
Cloudbyz Unified Clinical Trial Management (CTMS) is a comprehensive, integrated solution to streamline clinical trial operations. Built on the Salesforce cloud platform, our CTMS provides real-time visibility and analytics across study planning, budgeting, start-up, study management, and close-out. Cloudbyz CTMS can help you achieve greater efficiency, compliance, and quality in your clinical operations with features like automated workflows, centralized data management, and seamless collaboration. Contact us today to learn how Cloudbyz CTMS can help your organization optimize its clinical trial management processes.
To know more about the Cloudbyz Unified Clinical Trial Management Solution contact info@cloudbyz.com